American Indian infants in North Dakota, South Dakota and Minnesota are roughly twice as likely to die as white infants — a disparity health officials bemoan as “unacceptably high.”

Jodi Lutjens, a visiting nurse with the Indian Health Service, listens to Toshina Oneroad's daughter breathe during a visit at the mother's home in Sisseton, S.D. Oneroad is a patient in a visiting nurse program designed to prevent infant mortality. American Indians face a much higher risk of infant death than the general population. Patrick Springer / The Forum
SISSETON, S.D. — Toshina Oneroad’s infant daughter has sparkling eyes and a sunny disposition, but her tiny cough caught the nurse’s attention.Jodi Lutjens, a visiting nurse with the Indian Health Service clinic near here, 90 miles south of Fargo, took the infant’s temperature.Normal. A good sign.
At the tender age of 1 month, the baby is vulnerable to infection — just the sort of pitfall Lutjens is trying to avoid through prevention and education, the front line of defense against infant mortality.
Babies like Wocekiya Oneroad are especially vulnerable.
That’s because American Indian infants in North Dakota, South Dakota and Minnesota are roughly twice as likely to die as white infants — a disparity health officials bemoan as “unacceptably high.”
Visiting nursing programs like those enabling Lutjens’ efforts on the Sisseton-Wahpeton reserva tion, seek to cure the stubborn problem.
The regular home visits, ideally starting before the child is born, blend assessment of risks and health status of mother and child with intensive health and safety education.
Oneroad first met Lutjens at a birthing class days before delivering Wocekiya, which means prayer in Dakota and is pronounced Woe-chee-yah. Reaching the one-month milestone, which coincided with Lutjens latest home visit on a recent day, was significant; 42 percent of infant deaths in South Dakota occur during the critical first month.
The nurse took out her stethoscope and listened to the baby breathe. The lungs were clear, also reassuring. And the mother reported there was no sign of infection, despite the running nose.
Still, Lutjens advised Oneroad, who is a member of the Sisseton-Wahpeton tribe, to keep monitoring her baby’s temperature and get her in to the doctor if she develops a fever.
“Just keep an eye on things,” she said.
Their first visit came after Oneroad spotted an advertisement for Lutjens’ birth preparation class, just days before Wocekiya was born. The breathing and relaxation techniques made her labor more tolerable.
“That really made a difference,” said Oneroad, 24, who also has a 5-year-old daughter. “The breathing really helped.”
First home visit
Days after the baby was born, Lutjens made her first home visit. At birth, Wocekiya weighed a healthy 9 pounds, 1 ounce. “She looked good,” Lutjens said. “She had a very good checkup,” adding her weight had grown to 10 pounds, 13 ounces.
American Indian infants often face greater risks than those of the general population. They are more likely to be born prematurely, have teenage mothers, grow up in poverty, or have a mother who smoked or used alcohol or other drugs during pregnancy.
Another major risk factor: going to sleep and not waking up.
SIDS, or sudden infant death syndrome, and other sleep-related causes, occur at higher rates for American Indians than the general population.
A Minnesota study of American Indian infant mortality attributed half of the reviewed deaths to SIDS or other sleep-related causes during 2005-2007, including being suffocated when the baby is sleeping in bed with a parent and suffocated when the mother or father rolls over the child during sleep.
To guard against that, Oneroad has been provided with a special infant bed that nestles next to her own, preventing the risk of the mother “overlaying” the baby in her sleep.
“With Toshina there’s not risk factors here,” Lutjens said. “She’s doing what she should be doing. She’s doing everything right.”
For her part, Oneroad appreciates the support and advice Lutjens brings with her visits.
“This is really nice,” she said. “With a newborn, it’s hard to get out. It’s nice having Jodi come here.”
Second mother
Mary Becker considered herself a second mother to the infant nephew she helped nurture.
“It really affected me,” she said. “I was in the room when he was born. I took care of him a lot. I tried to be the helpful aunt.”
So after the boy’s death four years ago from SIDS, she vowed to do everything possible to avoid the same fate when she had a child of her own.
That time came more than two years ago, and Becker decided to leave the Turtle Mountain Indian Reservation in north-central North Dakota and move to Fargo.
She was 18 years old, and joined by her boyfriend, now her fiance. Both decided it would be easier to find work and housing in Fargo, where Becker had lived for a time with her father.
She also wanted to escape from an unhealthy family environment; her siblings had repeated their mother’s abuse of alcohol, and she didn’t want that contagion to spread to her child.
Program for mothers
A little more than two years ago, during a visit at the Family Healthcare Center in Fargo, she learned about a public health visiting nurse program for mothers who qualify according to income and other criteria.
She started on the program when she was five months pregnant.
“I’ve been with her ever since,” said Kara Scheer, a nurse with Fargo Cass Public Health’s Baby Steps Nurse-Family Partnership program.
On a recent rainy morning, Scheer met with Becker, 21, and her, Rockyboy Jr., 2. It was a graduation of sorts; this would be their last visit.
The nurse gave a glowing report card to mother and son.
“He’s just done amazing and she’s been amazing,” Scheer said. They’ve just done well through the whole process.”
As they sat on a sofa in Becker’s living room, with Rockyboy playing with wooden blocks, the nurse reviewed health and safety tips.
The Nurse-Family Partnership, a national program in use in both Cass and Clay counties, involves weekly in-home visits for up to 2½ years to guide first-time mothers through the critical period in child development.
The approach fosters good parenting skills and draws upon 30 years of evidence-based preventive health steps and education, with the nurse serving both as health professional and life coach.
On their last visit, Scheer takes final weight and height measurements. Rockyboy’s numbers fall squarely within the normal range.
As Toshina Oneroad found in Sisseton, having a nurse come into your home makes it easy to stay on track to keep the child healthy, Becker said.
“You’re in your own comfort zone,” she said. “You’re in your own home. I’ve learned so much,” including proper breastfeeding guidance and what to expect at each step of Rockyboy’s development.
“She actually taught me patience,” Becker added. “Between the program and the mother instincts kicking in, I could handle it.”
Baby Steps
Unfortunately, many American Indian mothers who have been in the Baby Steps visiting nurse program, who comprise 4 to 5 percent of the families served, have failed to finish, Scheer said. Many end up moving back to their home reservations.
Meanwhile, a collaboration between the White Earth and Fond du Lac Ojibwa bands in Minnesota could bring the Nurse-Family Partnership visiting nurse program to their reservations.
The two tribes have cooperated in a pilot study to adapt the national program, blending national standards and tailoring the approach to work better with Ojibwa culture.
So far, families have embraced the program. “Moms are engaging with that curriculum,” said Pat Butler, a nurse who manages the White Earth Home Health Agency.
Three nurses provide home visits for maternal and child health care, reaching between 40 and 50 families at a time.
Bringing the program to White Earth, located north of Detroit Lakes, Minn., is a priority of the tribe, Butler said.
“Your families are the future, guided by the elders,” she said.
If the Minnesota Ojibwe bands succeed in getting approval to modify the Nurse-Family Partnership program, they will become the first tribes to do so.
José Gonzalez, who directs a program of the Minnesota Health Department that works to end health disparities, said the collaboration between the White Earth and Fond du Lac bands is an example of how tribes are working to address infant mortality and other health problems.
The infant mortality rate for American Indians in Minnesota was 10.3 percent, compared to 4.4 percent for whites during 2001 to 2005, the most recent state comparison available.
Similar disparities were found in North Dakota and South Dakota, according to figures for 1999 to 2008 compiled by the Northern Plains Tribal Epidemiology Center, based in Rapid City, S.D.
In North Dakota, the infant mortality rate for American Indians is 11.9 percent, almost double the 6 percent rate for whites. In South Dakota, 13 percent of American Indian infants die, more than twice the 5.8 percent of whites.
North Dakota health officials are watching the experiment at Minnesota’s White Earth and Fond du Lac reservations.
“We’re aware of that pilot,” said Kim Mertz, director of the division of family health at the North Dakota Health Department. “We recognize we have to do a better job.”
Home visits
Nurse Jodi Lutjens started making maternal and child health home visits on the Sisseton-Wahpeton Dakota reservation three years ago.
She’s one of five visiting public health nurses with the Indian Health Service clinic in Sisseton, and the only one focusing on maternal and child health. She drove 14,000 miles to make her appointments last year.
Before Lutjens and several colleagues were hired, two visiting nurses tried to cover the entire service population, about half of the reservation’s 12,000 residents.
“I feel there’s been a big improvement in what I’ve seen,” she said, referring to infant mortality, which was 10.1 percent in Roberts County, the heart of the reservation, from 2000 to 2009.
“We’re still seeing infant deaths, but I’ve seen that number going down since I’ve been working here. We can’t prevent it entirely, but we can give education.”
Lutjens and her colleagues with the IHS collaborate with the tribe, including visiting home aides who can take mothers and children to their doctor’s visits.
As the nurse wraps up her visit with Oneroad, she remarks that she’s pleased that Wocekiya is eating well, and now weighs almost 11 pounds.
“This is just a case where mom and baby – they’re good,” she said. Then, turning to Oneroad, she adds, “We’ll be in touch.”
http://www.grandforksherald.com/event/article/id/208731/




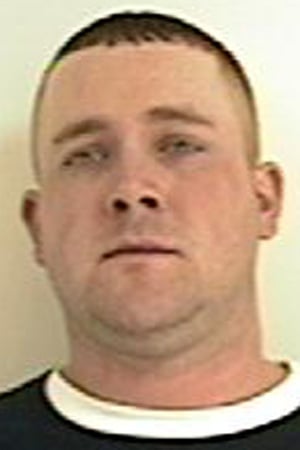
 Dustin James McCord, 22, was charged with aggravated child abuse after what police termed was an incident of shaken baby syndrome. A release from the police department said they had been contacted by staff at Erlanger hospital who said “a 5-month-old baby had been brought in suffering from a seizure and exhibiting past and present shaken-baby symptoms.”
Dustin James McCord, 22, was charged with aggravated child abuse after what police termed was an incident of shaken baby syndrome. A release from the police department said they had been contacted by staff at Erlanger hospital who said “a 5-month-old baby had been brought in suffering from a seizure and exhibiting past and present shaken-baby symptoms.” 